Current gold standard technique for tissue management in diabetic foot ulcers is regular sharp debridement to reduce bioburden, as this optimizes effectiveness of antimicrobials and stimulates wound healing.1 However, the extent of debridement required to reduce bioburden based on visual inspection is unclear, as point of care detection of bioburden relies primarily on visual inspection of wounds and subjective clinical signs and symptoms.2

Clinician's Testimonial
“Guiding debridement with the MolecuLight i:X reassured me that I was targeting regions of bioburden and avoiding unburdened tissue – which provided a more optimal state for wound healing.”
Rose Raizman, RN-EC, MSc, Scarborough & Rouge Hospital, Toronto, ON, Canada
Clinician Profile
With over 19 years of experience, Rose Raizman leads the Save Our Skin (SOS) team at Scarborough & Rouge Hospital located in Toronto, Canada, to combat pressure ulcers of hospital inpatients. She also oversees the wound care clinic for inpatients and outpatients.
Clinical Synopsis
Patient Condition: 57 year old male patient delayed seeking treatment for a diabetic foot ulcer on his left toe for more than 2 months. Some challenges with this wound included rapid callus build-up, improper footwear, delayed treatment, and a lack of offloading.
This patient treated their diabetic foot ulcer with an over-the-counter antibiotic ointment for two months prior to seeking treatment from a wound care practitioner. This patient’s lack of understanding of his condition, improper footwear, and delay of treatment were likely factors that led to infection.
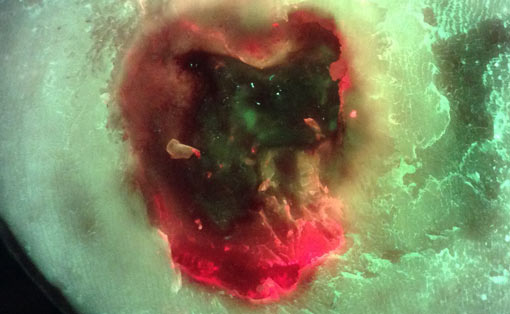
Pre-debridement, the clinician observed no red fluorescing bacteria (Figure 2). However, after debridement, the images revealed red fluorescence (Figure 4), indicating that there were indeed bacteria present in the wound.
 Image taken pre-debridement |
 Heavy callus pre-debridement, no red fluorescing bacteria observed |
|
 Image taken after debridement |
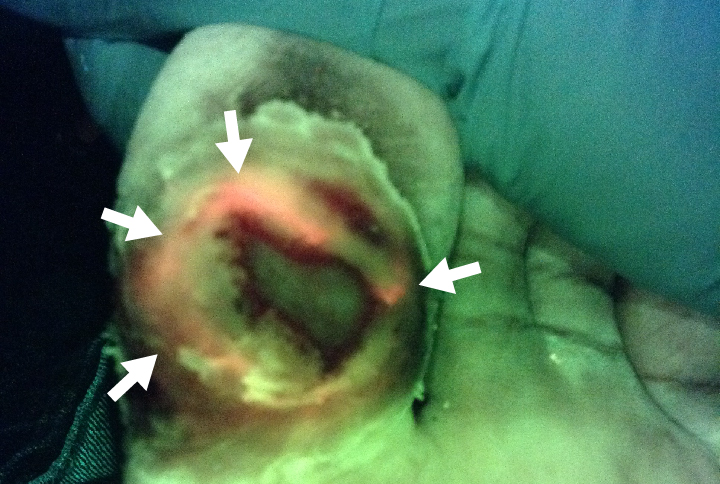 Initial debridement revealed red fluorescing bacteria |
|
The clinician then continued to debride using MolecuLight i:X guidance until the red fluorescing bacteria were no longer detected (Figure 6).
 |
 Wound debrided under MolecuLight i:X guidance until red fluorescing bacteria were no longer detected |
|
Using the MolecuLight i:X throughout treatment not only helped the clinician target debridement to areas of red fluorescing bacteria, but also emphasized the importance of regular debridement in a clinical setting.
The patient was shown images of his wound throughout the MolecuLight i:X guided debridement process, the simple image color scheme (green = tissue, red = bacteria), helped him better understand bacterial infection and the severity of his condition. Visual documentation of the wound’s progress also helped the clinician and patient observe the effectiveness of the treatment over time.
At a Glance
| Wound etiology & location | Diabetic foot ulcer, left foot, toe |
| Patient demographics | Male, 57 years old |
| Patient-related challenges |
Lack of patient awareness, delay of treatment ( > 2 months) Improper footwear, lack of offloading Rapid callus build-up requiring frequent debridement |
| Patient’s general care paradigm |
Weekly debridement Antimicrobial foam Offloading and local wound care |
| Clinician stated utility of the MolecuLight i:X |
Increase patient awareness of their condition Guided debridement |