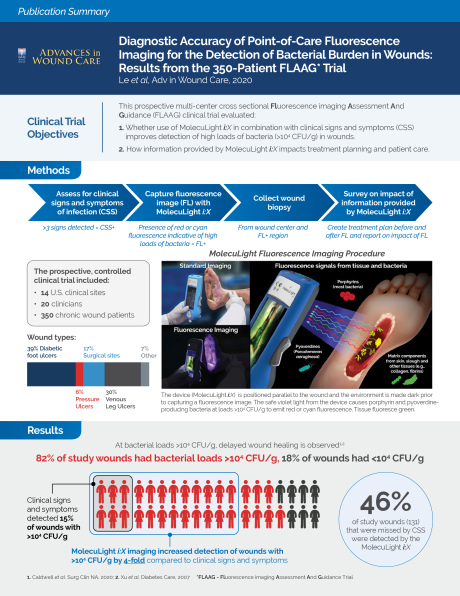
Abstract
Objective: High bacterial load contributes to chronicity of wounds and is diagnosed based on assessment of clinical signs and symptoms (CSS) of infection, but these characteristics are poor predictors of bacterial burden. Point-of-care fluorescence imaging (MolecuLight i:X fluorescence imaging device) can improve identification of wounds with high bacterial burden (>10<sup>4</sup> CFU/g). Fluorescence imaging detects bacteria, whether planktonic or in biofilm, but does not distinguish between the two. In this study, diagnostic accuracy of fluorescence imaging was compared to CSS during routine wound assessment. Post-assessment, clinicians were surveyed to assess impact of fluorescence imaging on treatment plan. Approach: A prospective multi-center controlled study was conducted by 20 study clinicians from 14 outpatient advanced wound care centers across the US. Wounds underwent assessment for CSS followed by fluorescence imaging. Biopsies were collected to confirm total bacterial load. 350 patients completed the study (138 diabetic foot ulcers, 106 venous leg ulcers, 60 surgical sites, 22 pressure ulcers, and 24 others). Results: 287/350 wounds (82%) had bacterial loads >10<sup>4</sup> CFU/g, and CSS missed detection of 85% of these wounds. Fluorescence imaging significantly increased detection of bacteria (>10<sup>4</sup> CFU/g) by 4-fold, and this was consistent across wound types (p<0.001). Specificity of CSS+ fluorescence imaging remained comparably high to CSS (p=1.0). Fluorescence imaging information modified treatment plans (69% of wounds), influenced wound bed preparation (85%), and improved overall patient care (90%) as reported by study clinicians. Innovation: This novel non-contact, handheld fluorescence imaging device (MolecuLight i:X) provides immediate, objective information on presence, location and load of bacteria at point-of-care. Conclusion: Use of fluorescence imaging facilitates adherence to clinical guidelines recommending prompt detection and removal of bacterial burden to reduce wound infection and facilitate healing.