ABSTRACT
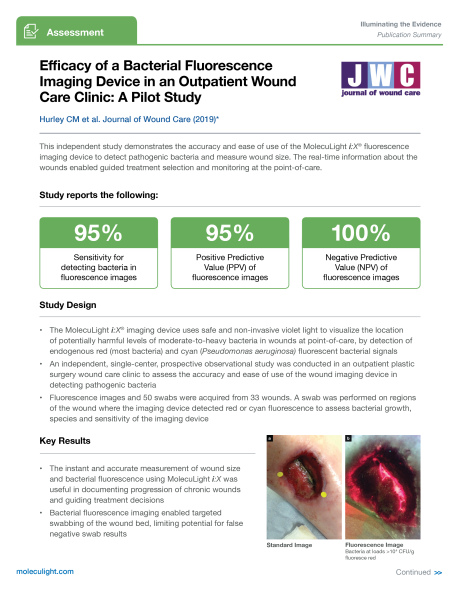
OBJECTIVE: Subsurface bacterial burden can be missed during standard wound examination protocols. The real-time bacterial fluorescence imaging device, MolecuLight i:X, visualises the presence of potentially harmful levels of bacteria through endogenous autofluorescence, without the need for contrast agents or contact with the patient. The intended use of the imaging device is to assist with the management of patients with wounds by enabling real-time visualisation of potentially harmful bacteria. The aim of this study was to establish the accuracy of the wound imaging device at detecting pathogenic bacteria in wounds.
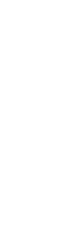
METHODS: A single-centre, prospective observational study was conducted in Cork University Hospital in an outpatient plastic surgery wound care clinic. Patients had their wounds photographed under white and autofluorescent light with the imaging device. Auto-fluorescent images were compared with the microbiological swab results.
RESULTS: A total of 33 patients and 43 swabs were included, of which 95.3% (n=41) were positive for bacteria growth. Staphylococcus aureus was the most common bacterial species identified. The imaging device had a sensitivity of 100% and specificity of 78% at identifying pathological bacteria presence in wounds on fluorescent light imaging. The positive predictive value (PPV) was 95.4%. The negative predictive value (NPV) was 100%. It demonstrated a sensitivity and specificity of 100% at detecting the presence of Pseudomonas spp.
CONCLUSION: The imaging device used (MolecuLight i:X) could be a safe, effective, accurate and easy-to-use autofluorescent device to improve the assessment of wounds in the outpatient clinic setting. In conjunction with best clinical practice, the device can be used to guide clinicians use of antibiotics and specialised dressings.