Abstract:
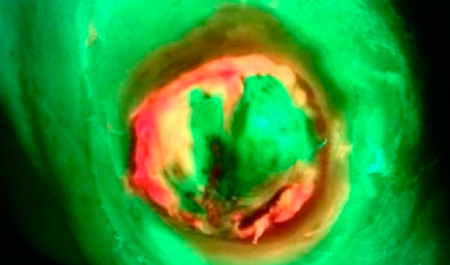
Objectives: To establish the clinical progression of dehisced perineal wounds healing by secondary intention and to investigate the incidence and factors associated with delayed healing. Methods: Secondary analysis of women with perineal wound dehiscence recruited into the PERINEAL study between August 2020- August 2021 (NCT 04480684). Three-dimensional wound measurements were taken with the Silhouette® camera. Significant bacterial colonisation was diagnosed using the MolecuLight i:X device. As it is agreed that acute wounds should heal sufficiently within four weeks, diagnosis of delayed wound healing was made if a wound took longer than four weeks to heal. A wound was deemed to have healed if there was complete wound closure, with no evidence of granulation tissue or signs of infection on clinical examination. Results: 55 women with perineal wound dehiscence participated. Wounds took an average of 3 weeks to heal (range 1–16) and 38 (69.1%) wounds healed in ≤ 4 weeks from the first clinical review. 17 (30.9%) wounds had significant bacterial colonisation, identified on bacterial fluorescence imaging. Women with a wound area of < 1.60 cm2 or wound perimeter of < 5.57 cm had a 70% probability of wound healing in ≤ 4 weeks. 47.1% of wounds with significant bacteria colonisation healed within 4 weeks, in comparison to 78.9% of wounds not colonised (p = 0.03). 25.0 % (n = 2) of wounds with OASI healed within 4 weeks, in comparison to 76.5% (n = 36) of wounds with no OASI (p = 0.02). Bacterial fluorescence (OR 0.21 (0.05–0.87)) and OASIs (OR 0.09 (0.01–0.66)) were independent risk factors associated with delayed wound healing. The model including wound area, fluorescence and OASIs had the greatest AUC (0.81, 95% CI 0.67–0.94) indicating the best predictive model. Conclusions: This is the first study to describe healing outcomes of dehisced perineal wounds and factors associated with delayed healing. The study findings will help clinicians counsel women effectively and tailor follow-up care at the first assessment, based on individual risk factors.