ABSTRACT
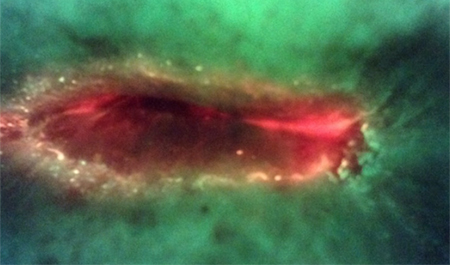
The urgent need to eliminate unnecessary use of antibiotics in wound patients has been hampered by diagnostic uncertainty and the time required to obtain culture results. The authors evaluated bedside use of a handheld bacterial fluorescence imaging device for real-time visualization of bacteria within and around wounds, used in addition to monitoring of clinical signs and symptoms of infection, in a series of 7 patients (5 women, 2 men; age range 57–93 years) with varying comorbidities who were referred to the wound ostomy continence clinician for wound assessment. When excited by 405-nm violet light, tissues fluoresce green (collagens) and bacteria fluoresce red; specialized optical filters reveal these colored signals in real time on the device’s display screen. Wounds exhibiting red fluorescence were presumed to have moderate/heavy bacterial contamination (≥104 CFU/g) and were subsequently swabbed. Swabs from the 5 wounds with regions of red fluorescence confirmed heavy growth of 1 or more pathogenic bacterial species. Images revealing pronounced bacterial fluorescence in 3 patients with pressure injuries about to be discharged led to prescription of systemic antibiotics and additional patient monitoring. In 2 patients (1 with a skin tear, 1 with a surgical wound), the absence of bacterial fluorescence prevented planned, unwarranted use of systemic antibiotics. Fluorescence images obtained bedside during routine wound assessments had a direct effect on antimicrobial stewardship practices. Follow-up images demonstrated antibiotic effectiveness and, in some instances, led to reduced antibiotic courses and duration. This case series demonstrates the potential use for real-time information on bacterial presence obtained via bacterial fluorescence imaging to guide evidence-based deployment of antibiotics and prevent unnecessary use. Additional studies to optimize the diagnostic potential and randomized controlled studies to examine the effect of this technique on antibiotic usage, antimicrobial stewardship practices, and wound outcomes are warranted.