Abstract:
Objective: Optimal wound-bed preparation consists of regular debridement to remove devitalised tissues, reduce bacterial load, and to establish an environment that promotes healing. However, lack of diagnostic information at point-of-care limits effectiveness of debridement.
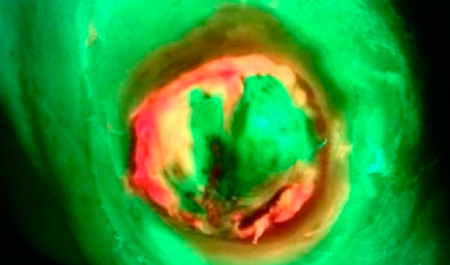
Method: This observational case series investigated use of point-of-care fluorescence imaging (MolecuLight i:X) to detect bacteria (loads >104CFU/g) and guide wound bed preparation. Lower extremity hard-to-heal wounds were imaged over a 12-week period for bacterial fluorescence and wound area.
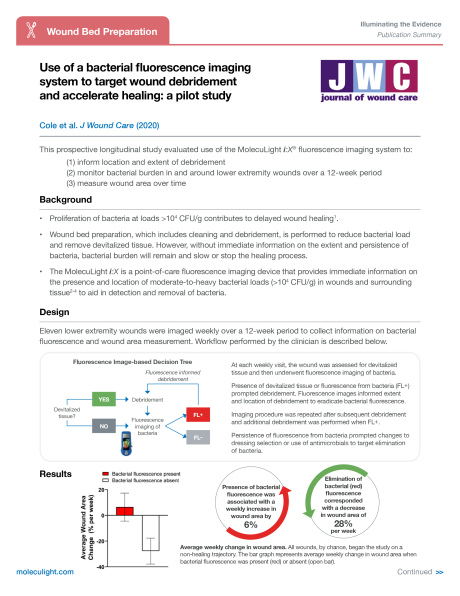
Results: A total of 11 wounds were included in the study. Bacterial fluorescence was present in 10 wounds and persisted, on average, for 3.7 weeks over the course of the study. The presence of red or cyan fluorescent signatures from bacteria correlated with an average increase in wound area of 6.5% per week, indicating stalled or delayed wound healing. Fluorescence imaging information assisted in determining the location and extent of wound debridement, and the selection of dressings and/or antimicrobials. Elimination of bacterial fluorescence signature with targeted debridement and other treatments correlated with an average reduction in wound area of 27.7% per week (p<0.05), indicative of a healing trajectory.
Conclusion: These results demonstrate that use of fluorescence imaging as part of routine wound care enhances assessment and treatment selection, thus facilitating improved wound healing.