ABSTRACT
Objective:
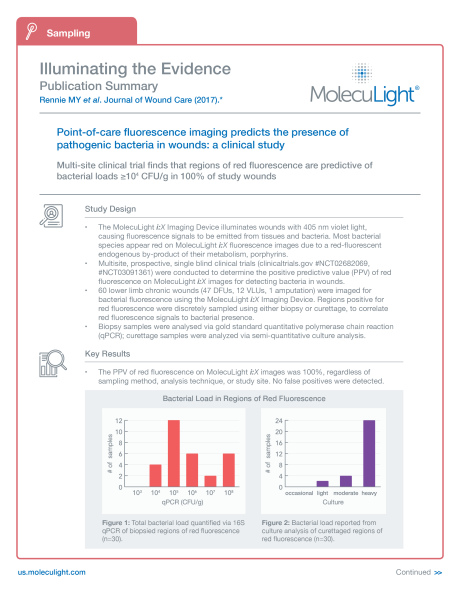
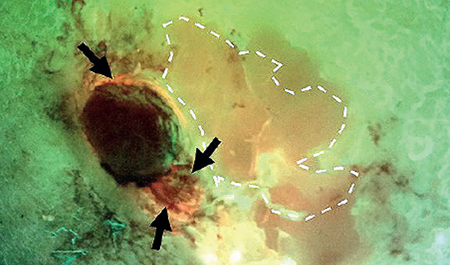
Bacteria in chronic wounds are invisible to the naked eye and can lead to delayed wound healing. Point-of-care bacterial fluorescence imaging illuminates a wound with 405 nm light, triggering bacteria to produce red fluorescence and enabling real-time bacterial localization. Prospective, single-blind clinical trials (clinicaltrials.gov #NCT02682069,#NCT03091361) were conducted to determine the positive predictive value (PPV) of this red fluorescence for detecting bacteria in chronic wounds.
Method:
Lower limb chronic wounds were imaged for bacterial fluorescence using the MolecuLight i:X Imaging Device. Regions positive for red fluorescence were discretely sampled using either biopsy (n=30) or curettage (n=30) to correlate red fluorescence signals to bacterial presence and analyzed via gold standard quantitative PCR (qPCR) or via semi-quantitative culture analysis respectively.
Results:
A total of 60 lower limb chronic wounds were imaged. qPCR analysis of wound tissue biopsies obtained from regions of red fluorescence yielded a PPV of 100 %. Total bacterial load in these areas was ≥ 104 CFU/g. Semi-quantitative culture analysis of curettage scrapings from regions of red fluorescence yielded a PPV of 100 %, with predominately moderate or heavy bacterial growth observed. There were nine distinct bacterial species were detected by red fluorescence, all common pathogens in chronic wounds. Staphylococcus aureus was the most prevalent species observed.
Conclusion:
Bacterial fluorescence image-guided curettage or biopsy sampling positively predicts bacterial presence in wounds at potentially harmful levels, entirely eliminating the risk of false negative sampling. Fluorescence imaging of wounds offers clinicians real-time information on a wound’s bacterial burden, insight which can influence treatment decisions at the point-of-care.