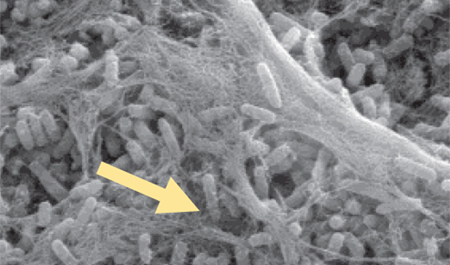
Objective: Approximately three million people in the US have hard-to-heal pressure ulcers (PUs), including 10% of hospitalised patients. Healing depends on ulcer stage and patient comorbidities. Despite advances in nutrition and wound care, PUs can take months or years to reach complete closure. To date, clinical studies have focused on single modality therapy. However, there is no one therapy that can address all of the deficits in these complex, hard-to-heal wounds. A commonly used treatment for PUs, negative pressure wound therapy (NPWT), has demonstrated improved healing in Stage 3 and 4 PUs. NPWT entails applying suction to a porous sponge fitted into the wound cavity and sealed with an occlusive dressing. Negative pressure facilitates wound healing by removing wound fluid containing harmful proteases, stimulating the formation of granulation tissue and promoting wound contracture. However, it does not affect biofilm formation. We hypothesised that adding an antibiofilm agent might increase the effectiveness of NPWT in recalcitrant PUs.
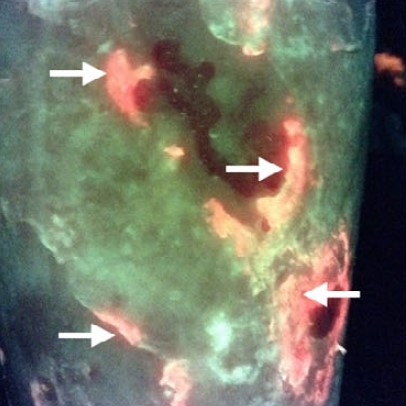
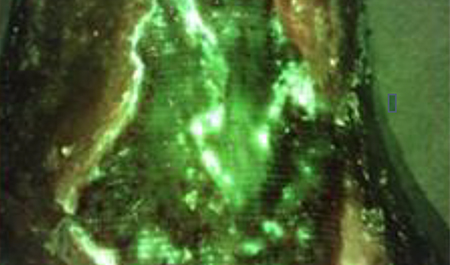
Method: A prospective case series was conducted in outpatient wound care centres and a skilled nursing facility to examine the combination of a biofilm-disrupting antimicrobial agent (Blast-X, Next Science, US) in combination with NPWT (VAC, 3M, US) in healing and reducing bacterial burden in treatment-resistant pressure ulcers. Patients consented to application of the antibiofilm agent and NPWT three times per week for four weeks. The wounds were measured, imaged for bacteria (MolecuLight i:X) and tested for host and bacterial protease activity weekly.
Results: Of the 10 patients, four dropped out of the study before the end of the four weeks. Of the remaining six, four patients experienced a reduction in wound surface area and volume, reduced protease activity and lower bacterial levels.
Conclusion: The results of this study showed that multimodal therapy, including NPWT and biofilm disruption, may restart the healing of stagnant treatment-resistant PUs.