MolecuLight significantly improved the detection of high bacterial load in each group of skin tones, peaking in the high group at 12-fold over CSS alone
MolecuLight is poised to provide a more objective and equitable indicator of wound bacteria
MolecuLight significantly improved the detection of high bacterial load in each group of skin tones, peaking in the high group at 12-fold over CSS alone
MolecuLight is poised to provide a more objective and equitable indicator of wound bacteria
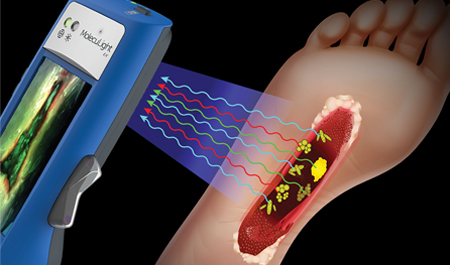
MolecuLight i:X helpful targeting for bacterial cultures as well as in judging therapeutic necessity for intractable skin ulcers.

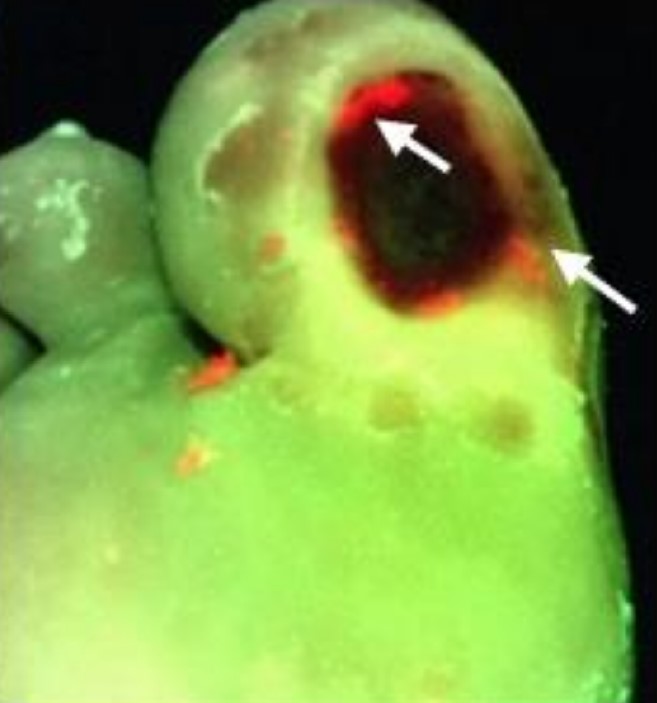
MolecuLight Improved Sensitivity 8.3-Fold for Detecting Bacterial Burden in DFUs over CSS alone
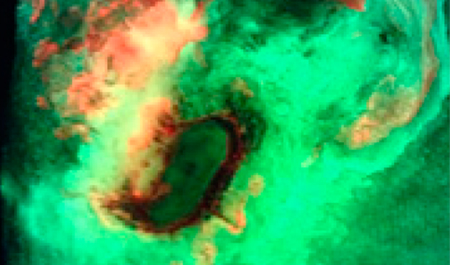
Fluorescence imaging showed that 84.2% of DFUs contained high bacterial loads in the periwound
Authors introduce new terminology, chronic inhibitory bacterial load (CIBL)

Quick detection of elevated bacterial burden enabled instant implementation of wound hygiene, skin disinfection, appropriate dressing choice and curative treatment was possible

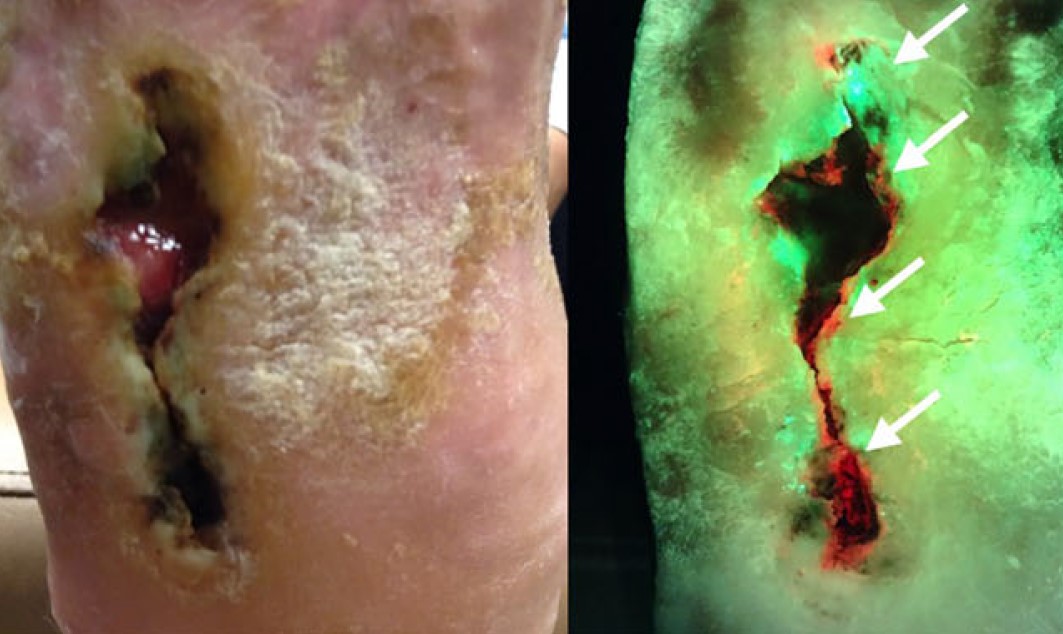
The use of MolecuLight to identify elevated bacterial loads in venous leg ulcers was confirmed and validated by pathology

Fluorescence imaging can help the specialist in a more targeted assessment and management of infection

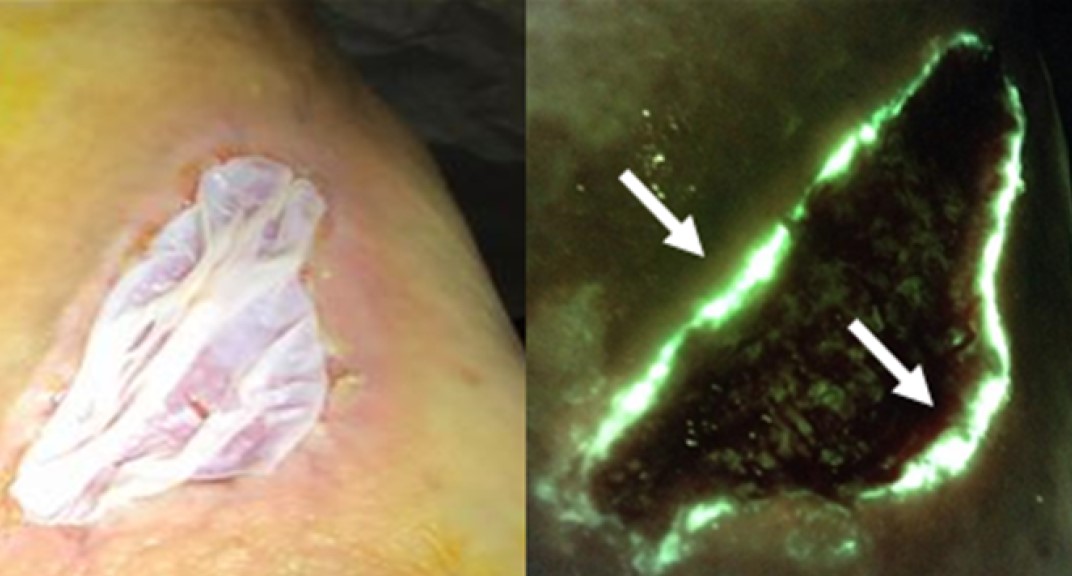
Fluorescent imaging excluded infection at the initial visit, and debridement was avoided
MolecuLight-assisted assessment of wound bacterial burden was helpful point-of-care tool in the clinician's armamentarium to diagnose pyoderma gangrenosum accurately

pH values on wound bed confirm non-invasive correlation between fluorescence & bacterial burden
MolecuLight i:X is able to objectively detect the bacterial proliferation in chronic wounds
MolecuLight also guides the correct assessment in the absence of clinical signs of infection and the presence of subclinical bacteria burden
Clinical signs and symptoms (CSS) assessment has poor sensitivity (6.8%) for detecting high bacterial loads in surgical wounds
Point-of-care fluorescence imaging for high bacterial loads improved sensitivity by 5.7-fold compared with CSS alone
Advanced image interpretation training, including hands-on experience, further increases sensitivity of fluorescence imaging up to 11.3-fold vs. CSS alone
Early awareness and management of bacterial burden & biofilm is essential to wound healing
Tissue biopsy & quantitative culture aren’t widely practiced and semi-quantitative analysis is unreliable
MolecuLight fluorescence imaging offers great potential to detect elevated bacterial burden in wounds
Delphi method was employed to establish consensus guidelines describing fluorescence imaging (MolecuLight i:X) use
96% reported that imaging-informed treatment plans led to improved wound healing
Guidelines provided will help to standardize use of fluorescence imaging among wound care providers

Advantage of utilizing point-of-care fluorescence imaging for improving bacterial detection and optimizing treatment strategies with wound sepsis in stage 4 pelvic pressure injuries.

MolecuLight i:X recommended, as review of NICE guidance in new JoWC publication "Wound healing: what is the NICE guidance from the UK?" for the assessment of fluorescent bacteria in wounds.
This review summarizes clinical evidence from the last 5 years evaluating the diagnostic accuracy and impact of adding fluorescence imaging to standard of care wound assessment
Several studies reported vast improvements in detection of bacterial burden in burn wounds with the addition of fluorescence imaging to standard of care
Incorporation of fluorescence imaging into patient care can change the trajectory of wound healing, leading to interventions that placed non-healing wounds on a healing trajectory
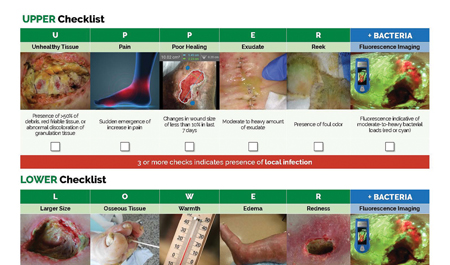
UPPER and LOWER CSS checklists were developed to distinguish between local & systemic infection
Addition of fluorescence imaging led to more judicious application of antimicrobials & more thorough wound bed preparation
95% sensitivity when fluorescence imaging was added over signs and symptoms alone (p<0.01)
69% of wounds had changes in treatment plans due to using the MolecuLight i:X
85% of wounds with wound bed preparation & high bacterial burden (>104 CFU/g) were impacted by information provided by the i:X
53% of wounds involving antimicrobial stewardship & high bacterial burden (>104 CFU/g) were impacted by information provided by the i:X

Hand trauma wounds were inspected for CSS and underwent fluorescence imaging for detection of bacterial burden
Fluorescence signals correlated with CSS and swab results in 97% of wounds
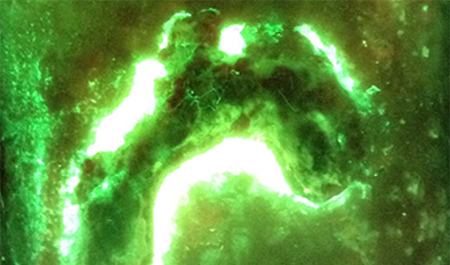
Fluorescence imaging can guide surgical debridement by providing real-time information on wounds' infected areas

The Fluorescence imaging procedure was used to inform advanced wound therapies
Three cases are described in which fluorescence images provided information at the point-of-care
This information was used to guide use of antibiofilm agents, NPWT, and preparation of the wound bed for grafting

This case series describes the utility of fluorescence imaging for detection of bacterial burden in an adult burn center
Fluorescence imaging informed decision making on dressings, antimicrobials and antibiotics used at point of care
Swabs confirmed accuracy of imaging results (positive or negative) in all 10 cases

Fluorescence imaging was used to monitor elevated bacterial loads during burn reconstruction
Weekly fluorescence imaging led to detection of elevated bacterial loads in the dermal template at the point-of-care
This resulted in debridement

Wounds were assessed for CSS & fluorescence images were then acquired to determine presence of moderate-to-heavy bacterial loads
Sensitivity of fluorescence imaging was 3-fold higher than CSS (72% vs 22%; p=0.002)
Fluorescence imaging information resulted in treatment plan modifications in 73% of study wounds
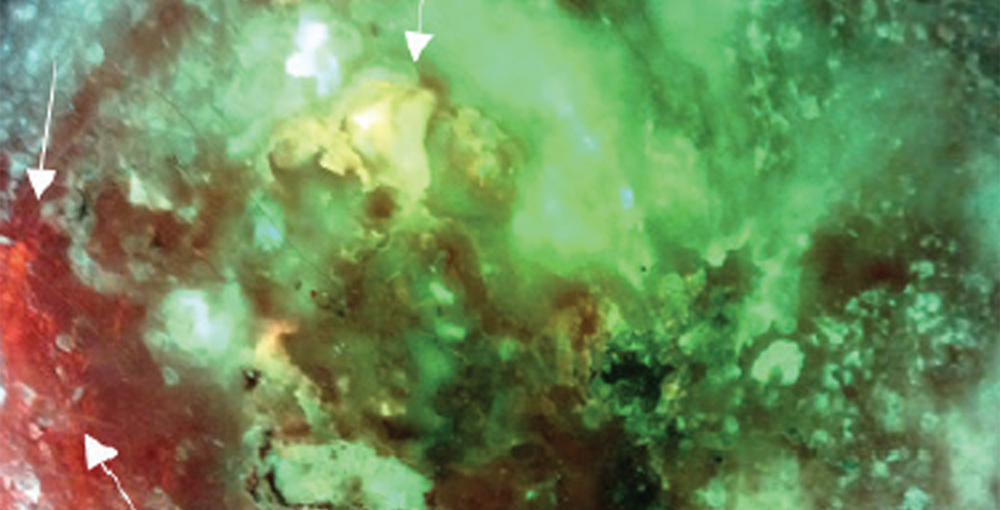
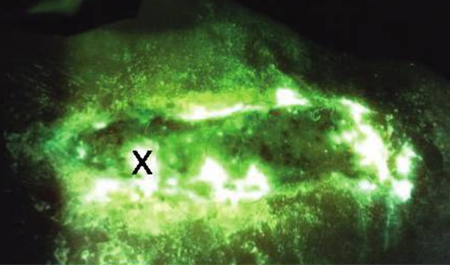
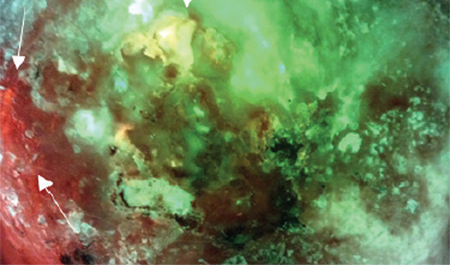
This peer-reviewed tutorial describes how to interpret the various fluorescence signals detected from wound tissues and bacteria using the fluorescence imaging procedure
Methods to minimize imaging artifacts and misinterpretation are described
Fluorescence images for identifying bacterial loads of concern was 100% vs 63% sensitivity of CSS
Fluorescence images for identifying bacterial loads of concern was 92% compared to 82% accuracy of CSS
Fluorescence correctly identified all 8 wounds that were positive for significant bacterial growth on cultures





A pre-clinical mouse wound model demonstrating the safety and feasibility of the fluorescence imaging procedure to visualize elevated bacterial burden in wounds
After treatment with antibiotics, bacterial fluorescence signal correlated with quantitative changes in wound bacterial load