Addition of MolecuLight to standard treatment doubled 12-week healing rates of DFUs (204%) and improved wound closure
Delphi method was employed to establish consensus guidelines describing fluorescence imaging (MolecuLight i:X use)
96% reported that imaging-informed treatment plans led to improved wound healing
Guidelines provided will help to standardize use of fluorescence imaging among wound care providers
23% increase in 12 week wound healing rate
33% decrease in antibiotic prescribing
47% decrease in antimicrobial spending per wound
69% of wounds had changes in treatment plans due to use of MolecuLight i:X
85% of wounds with wound bed preparation & high bacterial burden (>104 CFU/g) impacted by fluorescence info from i:X
53% of wounds involving antimicrobial stewardship & high bacterial burden (>104 CFU/g) impacted by fluorescence info from i:X

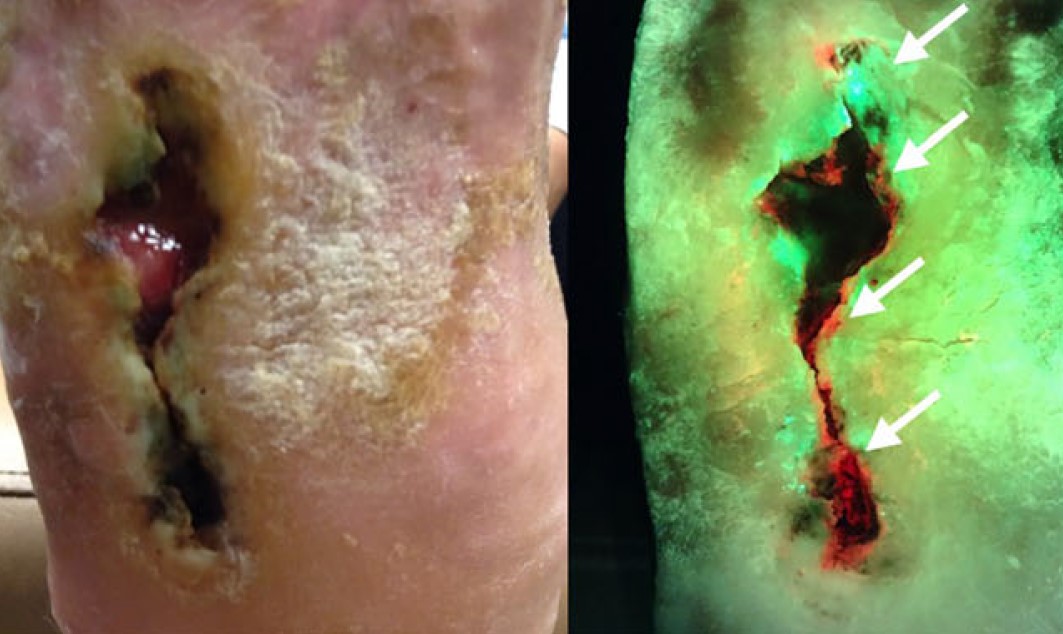
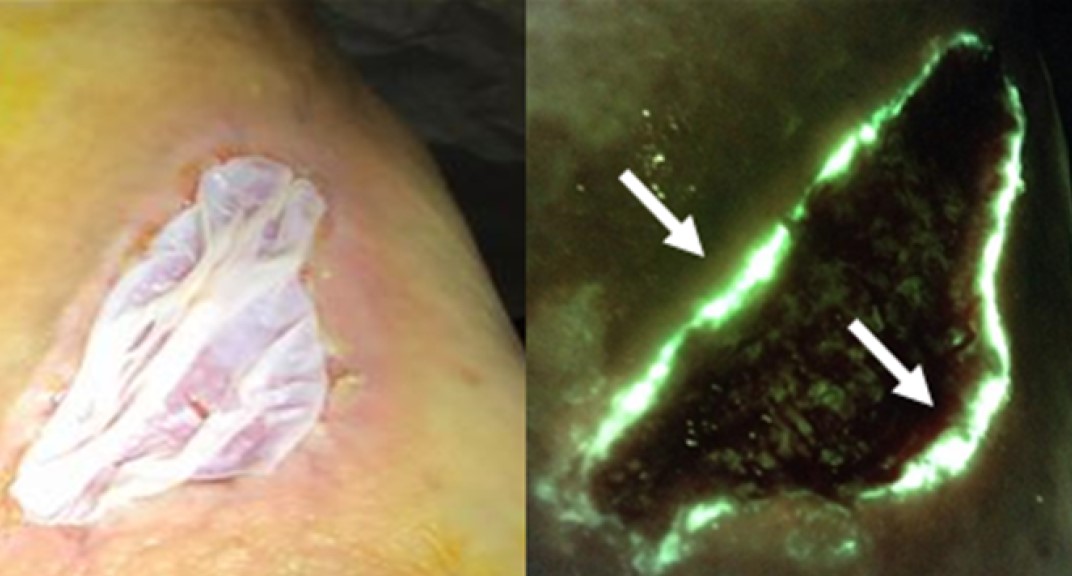
MolecuLight imaging is an important tool to help clinicians guide debridement and remove biofilm in venous leg ulcers (VLUs)

Repeated fluorescence imaging and targeted fluorescent-guided debridement (MolecuLight) was useful for managing bacterial bioburden to support wound healing

Real-time fluorescence imaging (MolecuLight) provides a novel and effective method along with the standard of care for managing osSSI after kidney transplantation
MolecuLight significantly improved the detection of high bacterial load in each group of skin tones, peaking in the high group at 12-fold over CSS alone
MolecuLight is poised to provide a more objective and equitable indicator of wound bacteria

Effective strategies include those that raise awareness of antibiotic overprescribing and those that enhance diagnosis of infection, such as fluorescence imaging (MolecuLight)
MolecuLight i:X helpful targeting for bacterial cultures as well as in judging therapeutic necessity for intractable skin ulcers.

Fluorescence imaging using MolecuLight provides a more accurate and relevant microbiological profile that guides optimal wound sampling compared to clinical judgment

MolecuLight Improved Sensitivity 8.3-Fold for Detecting Bacterial Burden in DFUs over CSS alone
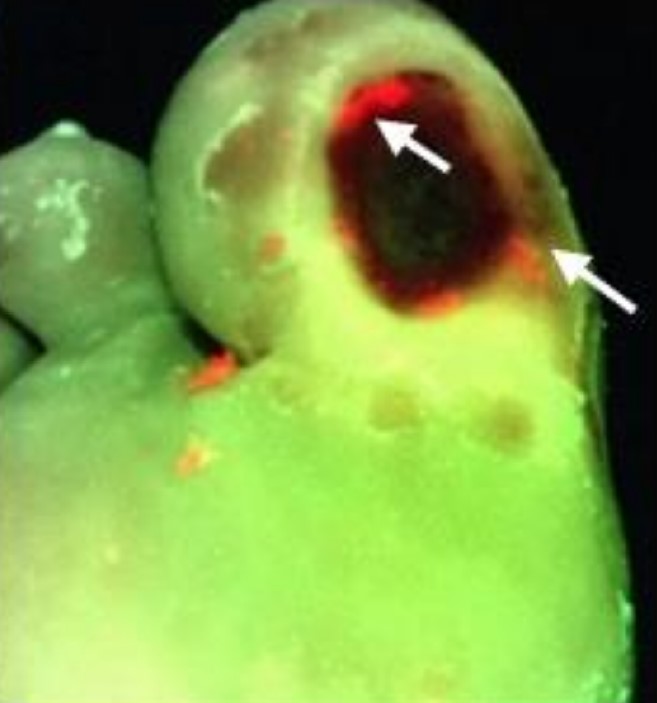
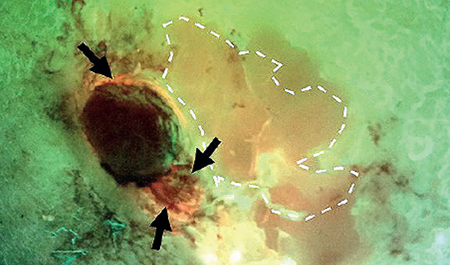
Fluorescence imaging showed that 84.2% of DFUs contained high bacterial loads in the periwound
Authors introduce new terminology, chronic inhibitory bacterial load (CIBL)

MolecuLight successfully used to detect location & load of elevated bacterial load prior to delivery of non-thermal gas plasma in DFU patients

Quick detection of elevated bacterial burden enabled instant implementation of wound hygiene, skin disinfection, appropriate dressing choice and curative treatment was possible

High diagnostic accuracy to detect elevated bacterial loads in perineal wounds
The sensitivity was 83%, specificity was 90%, and the PPV was 92%

In 33.3% of patients prescribed systemic antibiotics, no CSS were present. Prescribing patterns did not correlate with bacterial load
Reliance on CSS to diagnose clinically significant bacterial burden in chronic wounds leads to the haphazard use of antimicrobials
Improved methods of identifying bacterial burden and infection (e.g. MolecuLight) are needed to enhance antimicrobial stewardship efforts in wound care

The use of MolecuLight to identify elevated bacterial loads in venous leg ulcers was confirmed and validated by pathology

Effectiveness of Alprep Pad® for cleaning and debridement of DFUs was studied
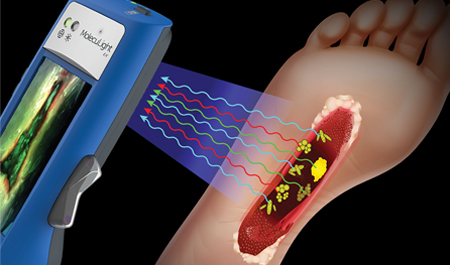
MolecuLight i:X was used to establish the presence of bioburden in the wound bed, wound edge and periwound skin
Wound size was measured using the MolecuLight device

First RCT using MolecuLight i:X technology
Addition of MolecuLight to standard treatment doubled 12-week healing rates of DFUs (204%) and improved wound closure

Fluorescence imaging aids antimicrobial stewardship by supporting evidence-based decision-making at the point of care
Also increased communication, enhanced efficiency, and improved continuity of care between wound care providers and hospital sites

1st study to describe healing outcomes of dehisced perineal wounds & factors associated with delayed healing
The presence of fluorescence significantly reduced the odds of wound healing in ≤ 4 weeks by 76%

Fluorescence imaging can help the specialist in a more targeted assessment and management of infection

Fluorescent imaging excluded infection at the initial visit, and debridement was avoided
MolecuLight-assisted assessment of wound bacterial burden was helpful point-of-care tool in the clinician's armamentarium to diagnose pyoderma gangrenosum accurately

pH values on wound bed confirm non-invasive correlation between fluorescence & bacterial burden
MolecuLight i:X is able to objectively detect the bacterial proliferation in chronic wounds
MolecuLight also guides the correct assessment in the absence of clinical signs of infection and the presence of subclinical bacteria burden

MolecuLight used in clinical trial of sodium hypochlorite to test its efficacy in reducing bacterial burden and promoting healing
Used to assess the presence of elevated burden in patients pre- and post-treatment
Initial findings: Sodium hypochlorite is efficacious in reducing bacterial burden and promoting healing
Clinical signs and symptoms (CSS) assessment has poor sensitivity (6.8%) for detecting high bacterial loads in surgical wounds
Point-of-care fluorescence imaging for high bacterial loads improved sensitivity by 5.7-fold compared with CSS alone
Advanced image interpretation training, including hands-on experience, further increases sensitivity of fluorescence imaging up to 11.3-fold vs. CSS alone

Reliance on CSS to diagnose clinically significant bacterial burden in chronic wounds leads to the haphazard use of antimicrobials
Improved methods of identifying bacterial burden and infection are needed to enhance antimicrobial stewardship efforts in wound care
MolecuLight i:X can provide utility in point-of-care detection of elevated bacterial burden
Efficient, accurate diagnosis of cellulitis critical to avoid costly complications
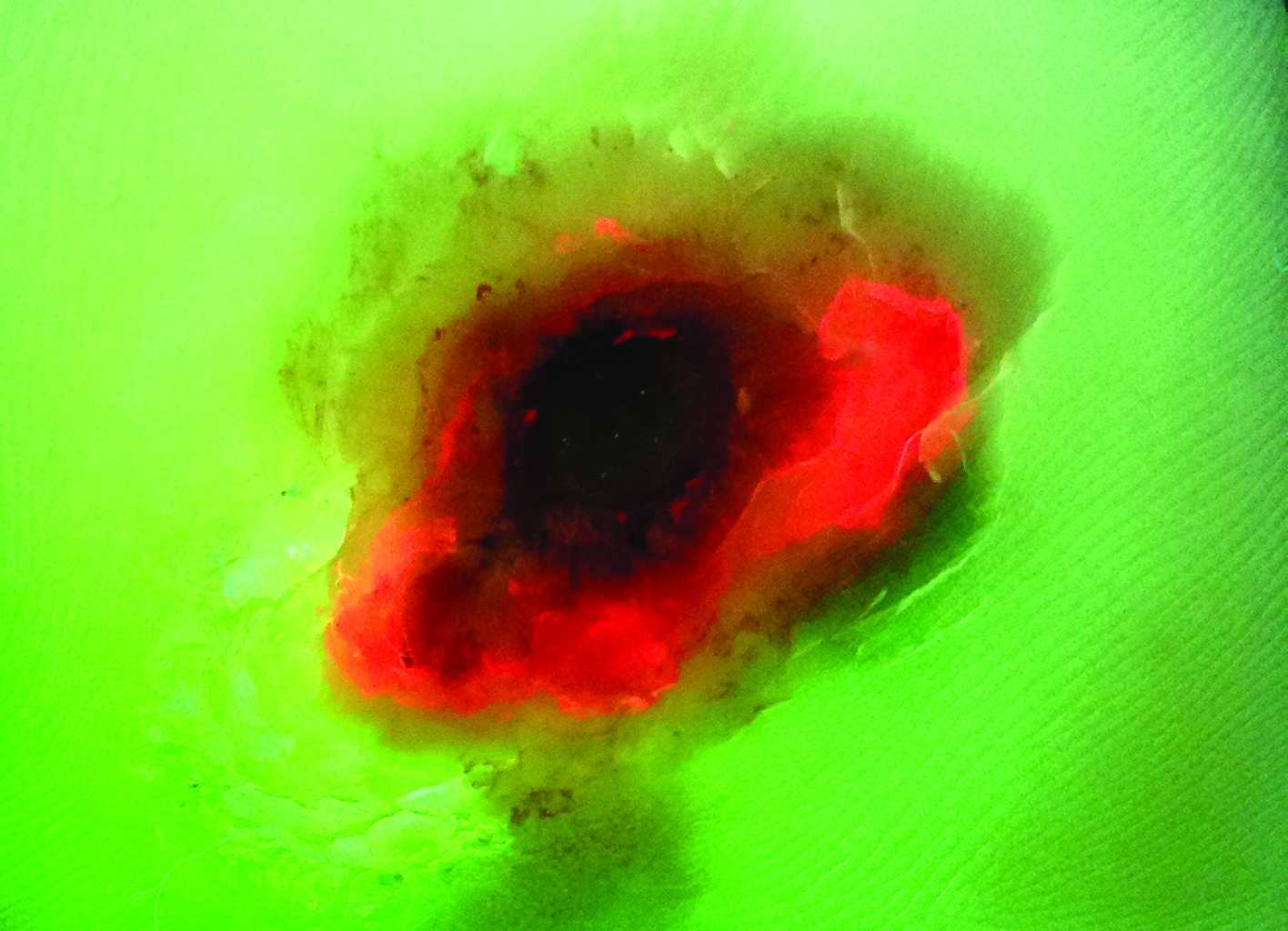
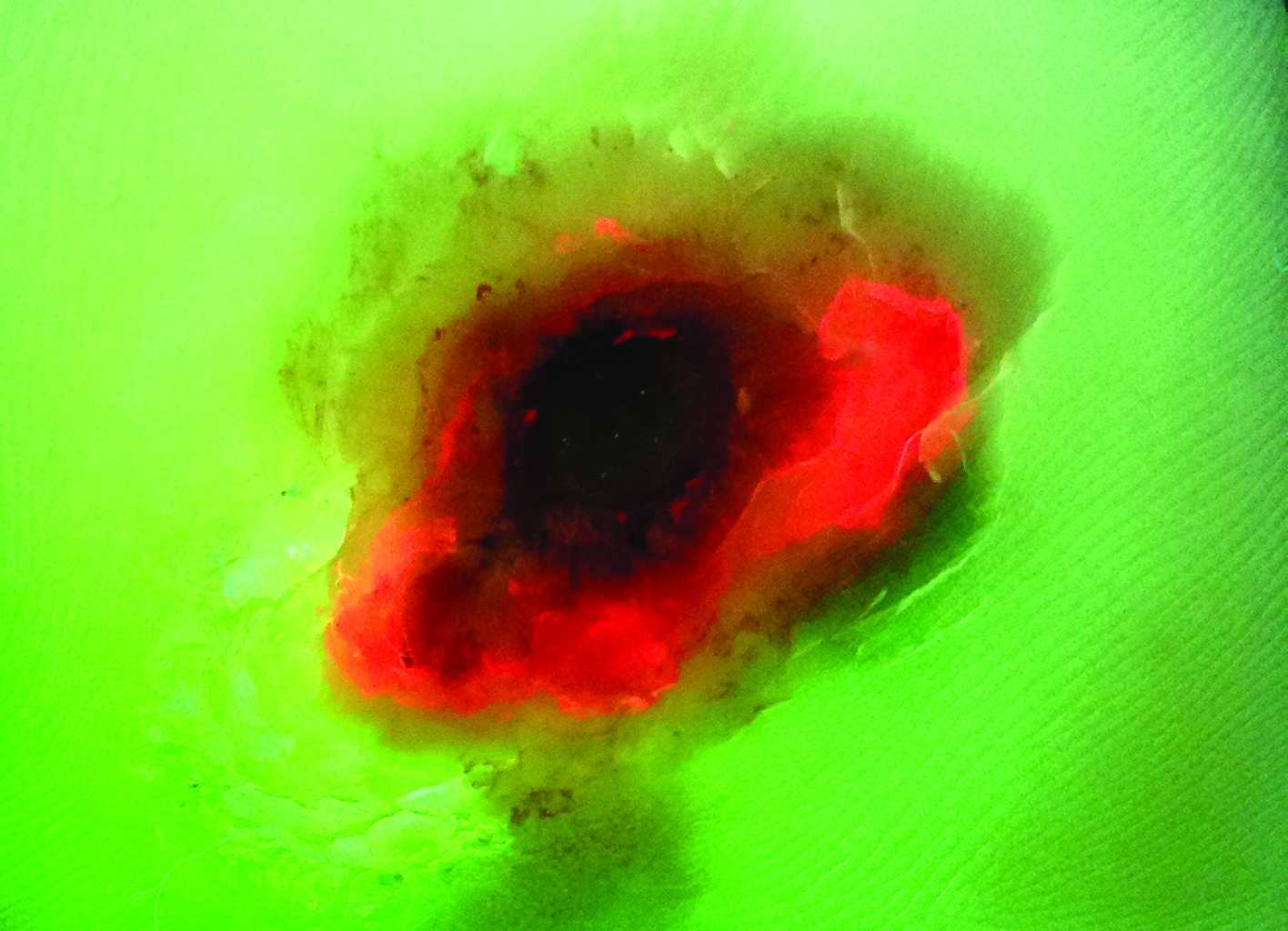
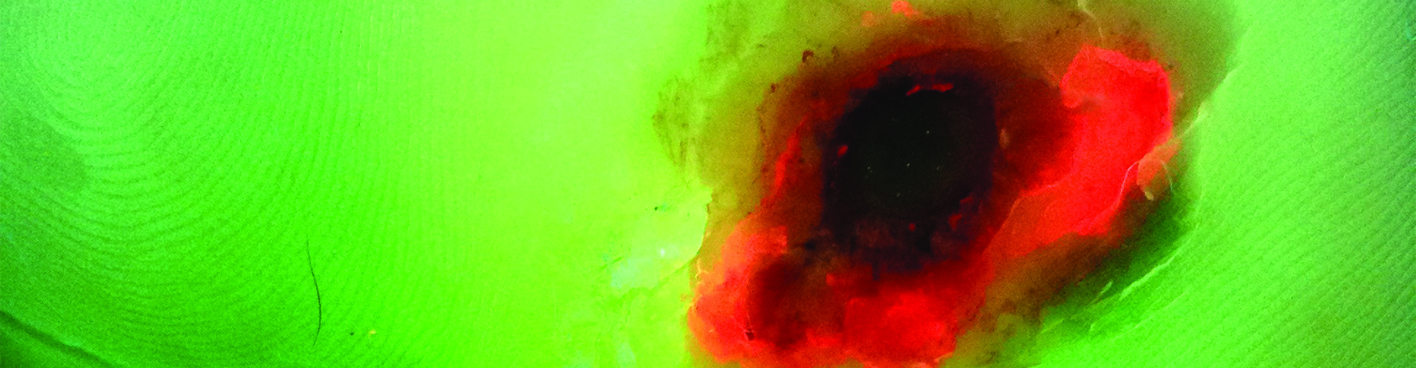
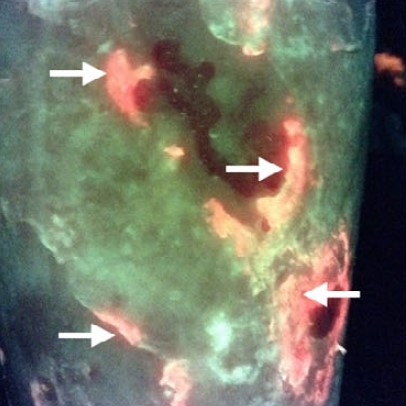
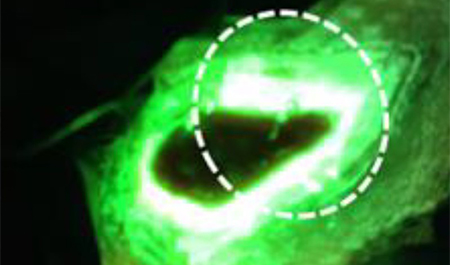
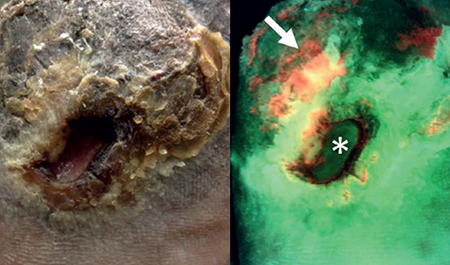
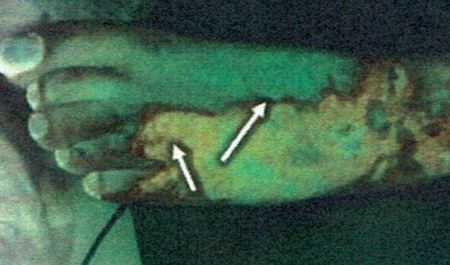
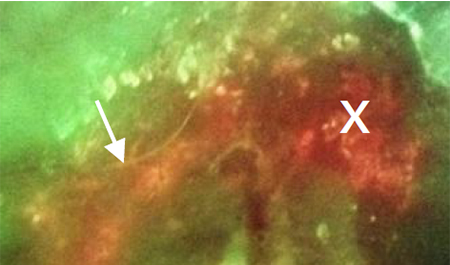
Unique pattern of red fluorescence extending beyond the wound was observed in all cases of wound-related cellulitis
Fluorescence imaging aided in the early diagnosis of wound-related cellulitis, resulting in the initiation of oral antibiotics without delay, avoiding progressive cellulitis
Early awareness and management of bacterial burden & biofilm is essential to wound healing
Tissue biopsy & quantitative culture aren’t widely practiced and semi-quantitative analysis is unreliable
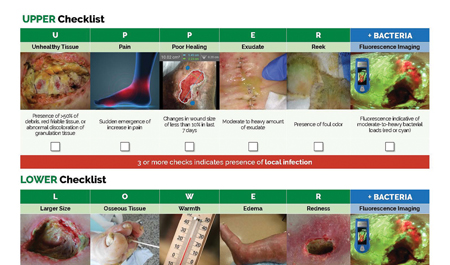
MolecuLight fluorescence imaging offers great potential to detect elevated bacterial burden in wounds
Delphi method was employed to establish consensus guidelines describing fluorescence imaging (MolecuLight i:X) use
96% reported that imaging-informed treatment plans led to improved wound healing
Guidelines provided will help to standardize use of fluorescence imaging among wound care providers

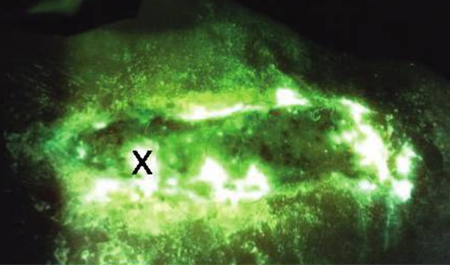
Using novel debridement tool, fluorescence imaging demonstrated a reduction in bacterial load in 69% of cases, with complete resolution in 19% of wounds.

Advantage of utilizing point-of-care fluorescence imaging for improving bacterial detection and optimizing treatment strategies with wound sepsis in stage 4 pelvic pressure injuries.

MolecuLight i:X recommended, as review of NICE guidance in new JoWC publication "Wound healing: what is the NICE guidance from the UK?" for the assessment of fluorescent bacteria in wounds.
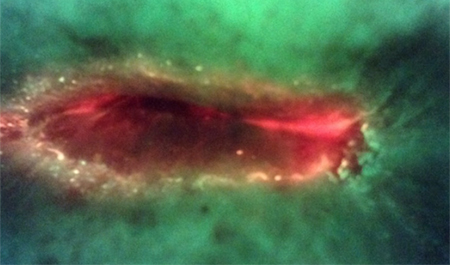
Pseudomonas aeruginosa, a common bacterial pathogen in chronic wounds, is challenging to detect by standard assessment of clinical signs and symptoms
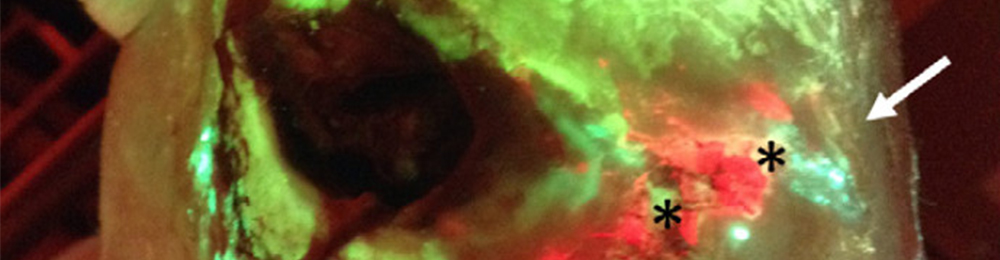
Cyan detected on MolecuLight i:X fluorescence images, can be used to reliably predict Pseudomonas aeruginosa at the point-of-care, with a PPV of 93% (confirmed by microbiological analysis)
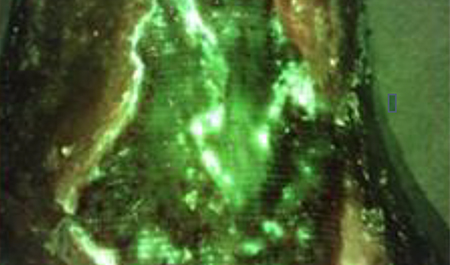
In this prospective trial, addition of a biofilm disrupting antimicrobial agent to NPWT reduced surface area and led to improved wound healing in 4/6 recalcitrant pressure ulcers
A reduction in wound area correlated with a reduction in bacterial burden as evidenced by fluorescence imaging (MolecuLight i:X)
The MolecuLight procedure enabled detection of bacteria build up in the NPWT sponges at the point-of-care
This review summarizes clinical evidence from the last 5 years evaluating the diagnostic accuracy and impact of adding fluorescence imaging to standard of care wound assessment
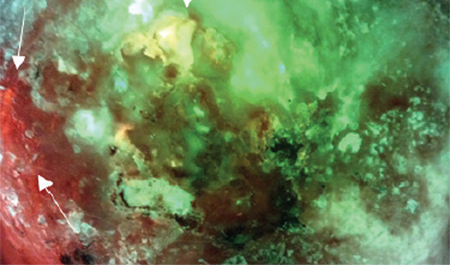
Several studies reported vast improvements in detection of bacterial burden in burn wounds with the addition of fluorescence imaging to standard of care
Incorporation of fluorescence imaging into patient care can change the trajectory of wound healing, leading to interventions that placed non-healing wounds on a healing trajectory

Successful removal of biofilm in wounds is contingent upon accurate detection of bacterial burden
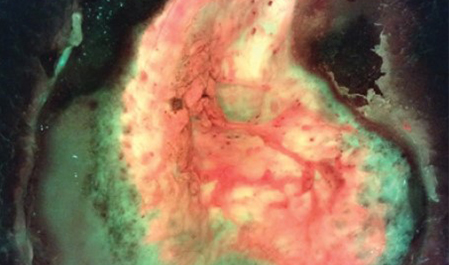
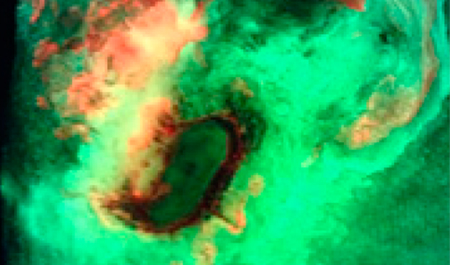
Fluorescence imaging (MolecuLight i:X) can detect wound bacteria encased in biofilm, as confirmed by SEM and histopathology
Red fluorescence observed from in vivo polymicrobial wound models is specific to bacteria, and not from an immune response
This study aimed to assess the efficacy and safety of a porcine peritoneum-derived matrix, a type of cellular and/or tissue product for treatment of DFUs
MolecuLight i:X imaging and measurement of bacterial protease activity (BPA) were performed weekly to evaluate bacterial load in wounds
Low bacterial loads, indicated by absence of fluorescence on MolecuLight i:X images and negative BPA, predicted wound healing

Fluorescence imaging was used to inform on the presence of bacterial loads in stage 3 and 4 pressure ulcers
These pressure ulcers underwent NPWT and treatment with a biofilm disrupting agent
In wounds where negative fluorescence images suggested lower bacterial levels, a reduction in wound surface area and volume was observed
Fluorescence imaging was used to meet Joint Commission guidelines for an antimicrobial stewardship program
Combined with clinical examination of signs and symptoms of infection, the MolecuLight imaging procedure improves the clinician’s ability to diagnose infection
Antimicrobial stewardship will soon become part of standard wound center reporting
23% increase in 12 week wound healing rate
33% decrease in antibiotic prescribing
47% decrease in antimicrobial spending per wound
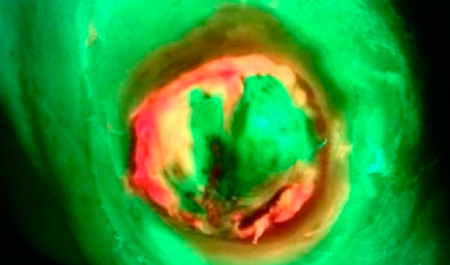
UPPER and LOWER CSS checklists were developed to distinguish between local & systemic infection
Addition of fluorescence imaging led to more judicious application of antimicrobials & more thorough wound bed preparation
95% sensitivity when fluorescence imaging was added over signs and symptoms alone (p<0.01)

This RCT used fluorescence imaging to evaluate the effects of cold atmospheric plasma on wound area of chronic wounds
Fluorescence images were used to visualize the bacterially colonized area and compare the area before and after
50.4 % reduction of bacterial load for Group 1 and 35.0 % for Group 2 compared to the day of study
69% of wounds had changes in treatment plans due to using the MolecuLight i:X
85% of wounds with wound bed preparation & high bacterial burden (>104 CFU/g) were impacted by information provided by the i:X
53% of wounds involving antimicrobial stewardship & high bacterial burden (>104 CFU/g) were impacted by information provided by the i:X

25% decrease in wound area over 4 weeks with the elimination of bacterial fluorescence from wounds
A positive healing trajectory was associated with the implementation of fluorescence imaging (i:X)
All wounds where fluorescence signal from bacteria was eradicated healed within 2-6 weeks

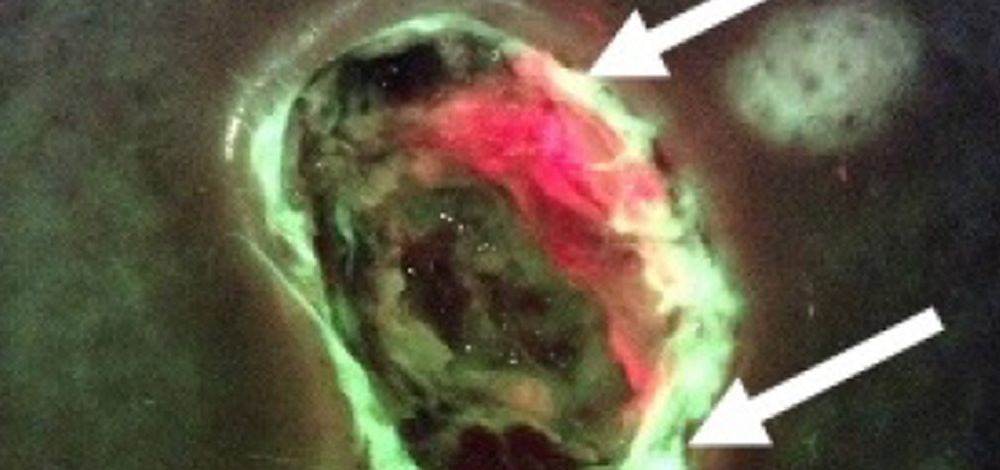
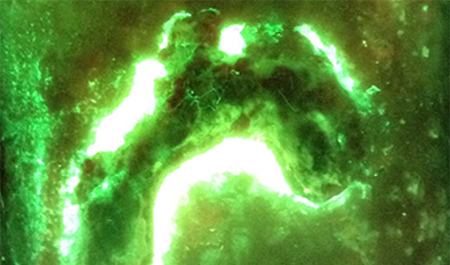
24% of VLU periwound area was colonized by high bacterial loads pre-debridement
99% reduction of bacterial signal in the wound bed after debridement using fluorescence guidance
36% of periwound bacterial signal is left behind after standard debridement in VLUs (without
the guidance of fluorescence)

Hand trauma wounds were inspected for CSS and underwent fluorescence imaging for detection of bacterial burden
Fluorescence signals correlated with CSS and swab results in 97% of wounds
Fluorescence imaging can guide surgical debridement by providing real-time information on wounds' infected areas

The Fluorescence imaging procedure was used to inform advanced wound therapies
Three cases are described in which fluorescence images provided information at the point-of-care
This information was used to guide use of antibiofilm agents, NPWT, and preparation of the wound bed for grafting
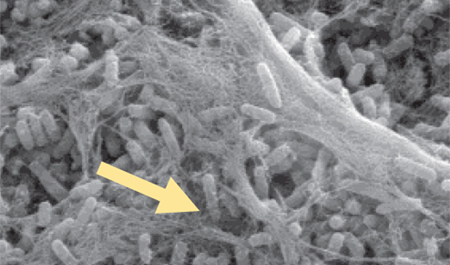
Fluorescence imaging (MolecuLight i:X) can detect both planktonic & biofilm bacterial cultures
Biofilm is present in more than 70% of chronic wounds and it contributes to delayed healing
Using fluorescence imaging to localize bacteria may facilitate targeted disruption of biofilm & bacterial removal
In a clinical trial with 412 punch biopsies, only one resulted in an adverse event (abscess)
Fluorescence images revealed presence of bacteria at site of biopsy prior to abscess development
Bacterial load was confirmed as 106 CFU/g from the biopsy

This case series describes the utility of fluorescence imaging for detection of bacterial burden in an adult burn center
Fluorescence imaging informed decision making on dressings, antimicrobials and antibiotics used at point of care
Swabs confirmed accuracy of imaging results (positive or negative) in all 10 cases
>95% measurement accuracy of MolecuLight i:X device for wound area, length and width
89% of wounds with red or cyan fluorescence in the periwound, a region rarely sampled
85% of DFUs where additional debridement was performed based on fluorescence guidance

Fluorescence imaging was more accurate than clinical judgement in detecting elevated bacterial loads
$7,660 USD per patient was the estimated cost savings from using fluorescence imaging information
This information avoided the application of cellular tissue products on wounds with high levels of bacteria

Fluorescence imaging was used to monitor elevated bacterial loads during burn reconstruction
Weekly fluorescence imaging led to detection of elevated bacterial loads in the dermal template at the point-of-care
This resulted in debridement


88% of wounds where bacterial fluorescence was detected in peripheries (in regions not typically swabbed)
100% of pediatric patients were compliant with the MolecuLight imaging procedure
93% of clinicians who reported highest practicality of incorporating MolecuLight i:X into routine diagnostic practice

9/10 wound care patients more appropriately triaged with fluorescence information
60% of these 9 patients would have been undertreated while 30% of patients were being overtreated
$1552 Single patient cost savings (USD) due to fluorescence evidence-based treatment plan changes
Wounds were assessed for CSS & fluorescence images were then acquired to determine presence of moderate-to-heavy bacterial loads
Sensitivity of fluorescence imaging was 3-fold higher than CSS (72% vs 22%; p=0.002)
Fluorescence imaging information resulted in treatment plan modifications in 73% of study wounds

95% Sensitivity for detecting bacteria in fluorescence images
95% Positive Predictive Value (PPV) of fluorescence images
100% Negative Predictive Value (NPV) of fluorescence images
This peer-reviewed tutorial describes how to interpret the various fluorescence signals detected from wound tissues and bacteria using the fluorescence imaging procedure
Methods to minimize imaging artifacts and misinterpretation are described

Estimated costs of a skin grafting procedure which was avoided based on real-time information from the i:X fluorescence images
Hospital stay (5 days) £2000
Operating room £1500
Fluorescence imaging was used to screen wounds treated with split thickness grafts
These wounds were processed by MEEK/MESH technique for bacterial burden
Fluorescence imaging shows high concentrations of pathogens both in the MEEK silk layer as well as in foam linkers

Fluorescence images provided the clinician with a “map” to inform wound sampling, cleaning, and location of surgical debridement
Heavy bacterial load was confirmed by microbiology methods in all wounds exhibiting red fluorescence
Fluorescence images identified asymptomatic patients and highlighted areas of clinical concern that otherwise would have been overlooked
The MolecuLight i:X aided clinicians in their management of wound infections
This was done through image informed debridement/treatment response monitoring to debridement & other wound therapies
Bacterial presence or absence based on fluorescence images correlated with swab results in all cases
Fluorescence images for identifying bacterial loads of concern was 100% vs 63% sensitivity of CSS
Fluorescence images for identifying bacterial loads of concern was 92% compared to 82% accuracy of CSS
Fluorescence correctly identified all 8 wounds that were positive for significant bacterial growth on cultures
The PPV of red fluorescence on MolecuLight i:X images was 100%, regardless of sampling method, analysis technique, or study site
Fluorescence guidance, in combination with subsurface sampling techniques, could eliminate the risk of false negative wound sampling
Fluorescence imaging information could influence treatment decisions at the point of care

Fluorescence imaging of diabetic foot ulcers had superior accuracy (78%) in detecting the presence of clinically significant bacteria than standard practice (Levine swabbing, 52%; p=0.048)
Higher bacterial loads were detected from wound regions positive for bacterial fluorescence compared to regions sampled based on CSS alone

This is an initial evaluation of using the MolecuLight i:X in the management of burns
The utility and efficacy of the MolecuLight i:X is evident due to the correlation between microbiology results and fluorescence images
The i:X may be able to detect bacterial load before an infection & subsequent graft failure, thereby shortening lengths of hospital stay & improving overall healing




A pre-clinical mouse wound model demonstrating the safety and feasibility of the fluorescence imaging procedure to visualize elevated bacterial burden in wounds
After treatment with antibiotics, bacterial fluorescence signal correlated with quantitative changes in wound bacterial load